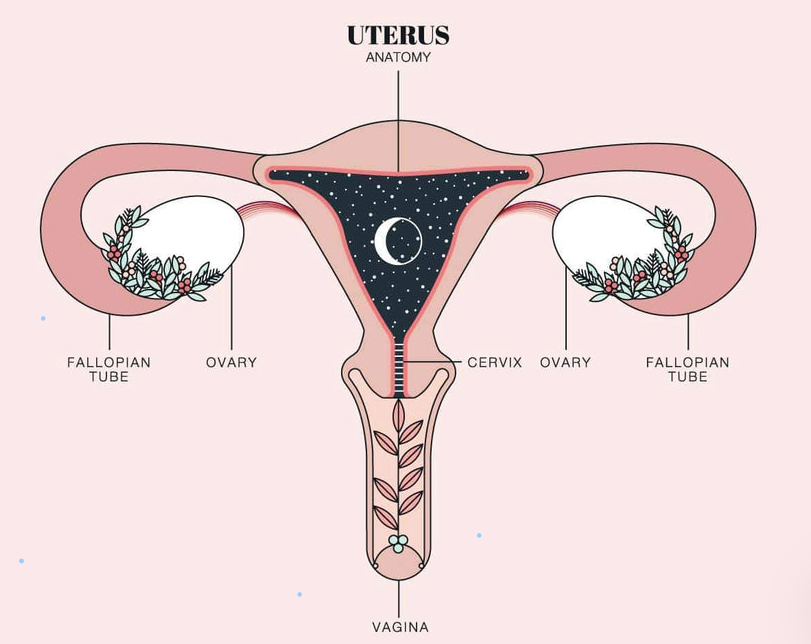
Understanding the menstrual cycle can often feel very complex and overwhelming. The graphs and anatomical drawings can sometimes feel like you’re just looking at a bunch of squiggly lines which resemble a mountain more than anything else, or even a smiley face holding golf balls on either side [insert clipart picture of uterus] Or is it just me or … ? It’s only much later in my studies did I come to realise how incredibly sophisticated the menstrual cycle is. This has certainly empowered me in being able to make decisions relating to my menstrual cycle, choice of contraceptives, understanding my period-related symptoms a little more, and even exercise routines that suit me at different times during my cycle.
First things first, your menstrual cycle is not just your period. If anything, it’s an incredibly dynamic hormone*-driven system that involves a series of activities in the brain, ovaries and uterus. Each month a woman’s body goes through multiple changes in order to prepare for and support a potential pregnancy. The menstrual cycle occurs during the years between puberty when you experience your first period (menarche) and continues up until menopause (when you have complete cessation of your period for at least 12 months).
*hormones: chemical messengers that travel in the blood
So what is your menstrual cycle then?
The menstrual cycle can be broken up into two smaller cycles: the ovarian and uterine cycles. Even though these cycles are often explained as two separate entities, their events typically overlap, and they’re intrinsically connected to one another.
Broadly speaking, the menstrual cycle occurs in 4 phases (menstruation, follicular, ovulation and luteal phases) which occur in either the first or second half of the cycle. Each phase is characterised by specific changes happening in the ovaries (ovarian cycle) and the uterus (uterine cycle).
First half of menstrual cycle
During the first half of your cycle, 3 phases occur:
- Menstruation: starts from day 1 of your period and marks the start of your new cycle.
- The duration of your period can range anywhere between 3 – 7 days. Some experts even argue that up to 9 days may be considered normal.
- Follicular phase: occurs from the last day of your period until ovulation.
- During this phase, oestrogen levels gradually rise as a premature egg undergoes maturation and growth.
- Oestrogen plays a major role in making the uterine lining (endometrium) “thick and spongy” in preparation for attachment (implantation) of a potentially fertilized egg.
- Once oestrogen levels peak this precipitates a sudden surge in a hormone released from the brain. This then triggers the release of the developed egg from the ovary [enter ovulation].
- Ovulation: the developed egg is released from your ovaries and into the fallopian tubes of the uterus (they often look like the short stumpy arms holding the golf balls in anatomical drawings)
- Typically happens midway through your cycle between days 12 -16 (aka your “fertile window”).
A little extra info on ovulation: even in people with relatively predictable periods, ovulation does not necessarily happen on the same day every cycle. Sometimes, ovulation may not even occur. This is called anovulation, which can be one of the reasons for an ireegular cycle. This can happen during your first few years of menstruation (remember that unexpected period during class – sigh…) and as your reproductive years start coming to an end (perimenopause). Other reasons for anovulation are pregnancy, breastfeeding, or certain conditions such as polycystic ovarian syndrome (PCOS). Without ovulating, it is unlikely that you will have a period in that cycle, but it still is not impossible.
Aside: Hormonal imbalances during different phases of your cycle can contribute to symptoms such as period cramps, acne, premenstrual syndrome, irregular cycles, and even no ovulation just to name a few.
If your cycle is persistently irregular, then I do advise you to consult a healthcare practitioner to explore the possible causes of your irregular cycles.
Second half of menstrual cycle
The fourth phase:
- Luteal phase: this starts after ovulation and continues until your next menstrual bleed. During this phase, progesterone levels rise while oestrogen slowly decreases. These two hormones act together to maintain the thick and spongy nature of the endometrium.
- If the released egg is not fertilized between 9 – 11 days after ovulation, it disintegrates, and progesterone levels rapidly decline. The endometrium lining starts detaching itself from the wall of the uterus and is shed out of your body as your period. You have now entered your next cycle – and these events happen all over again.
I hope that this brief overview of your menstrual cycle has made you understand that your cycle is more than just your period, and that variation in your cycle is normal (remember your body is not a clock). Understanding your menstrual cycle and keeping track of the changes your body is undergoing can help you to understand why you are experiencing certain symptoms, assist in preventing or planning for pregnancy, and most importantly it fosters an empowering and deep relationship between you and your body.
Disclaimer: This article is for informational purposes only. It is not, nor is it intended to be, a substitute for professional medical advice, diagnosis, or treatment and we recommend that you always consult with your healthcare practitioner.
Nokukhanya Zondi - final year Medicine student (MbChB), University of Cape Town